All masks are not created equal
Michigan Engineers test to evaluate safety.
Michigan Engineers test to evaluate safety.
N95 respirator masks that protect healthcare workers and patients from COVID-19 continue to be a valued but finite commodity—forcing some medical facilities to disinfect and reuse them, as well as go outside their normal, trusted routes for supplies.
That creates an air of uncertainty around masks being used by many on the front lines of the pandemic. University of Michigan engineers and physicians have created a testing system to evaluate the effectiveness of N95 and surgical masks for Michigan Medicine and several outside facilities, including a Battle Creek hospital.
Researchers have examined:
Early findings have confirmed that new N95 respirator masks obtained outside normal channels, as well as those that have been disinfected, meet standards set by National Institute for Occupational Safety and Health (NIOSH). Most of the imported KN95 masks also performed well, but a small number of new imported respirators that were tested did not. Surgical masks have generally produced positive test results.

“There’s too many people scrambling for those certified masks and rather than go without any mask at all, they’re now getting them from other sources, sometimes other countries,” said Herek Clack, a U-M associate professor of civil and environmental engineering. “And so then the question arises—can we be sure that these masks are performing as well as the ones we would normally get?”
Clack and Mirko Gamba, a U-M associate professor of aerospace engineering, have tested roughly 100 masks so far. Samples from one batch of KN95 masks failed to meet the NIOSH bar of filtering out at least 95% of airborne particles.
The quality of masks and other personal protective equipment is increasingly becoming an issue. Earlier this month, manufacturer 3M sued one distributor on Amazon selling fake N95 masks for well over their value. In May, the state of Texas rejected 200,000 masks from one vendor after finding faults with them.
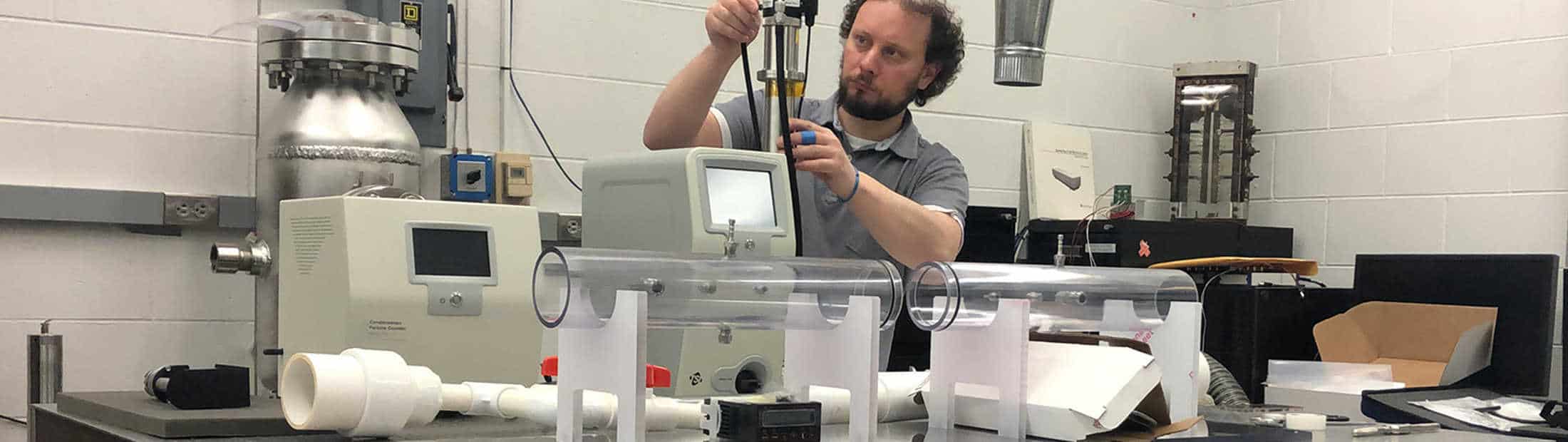
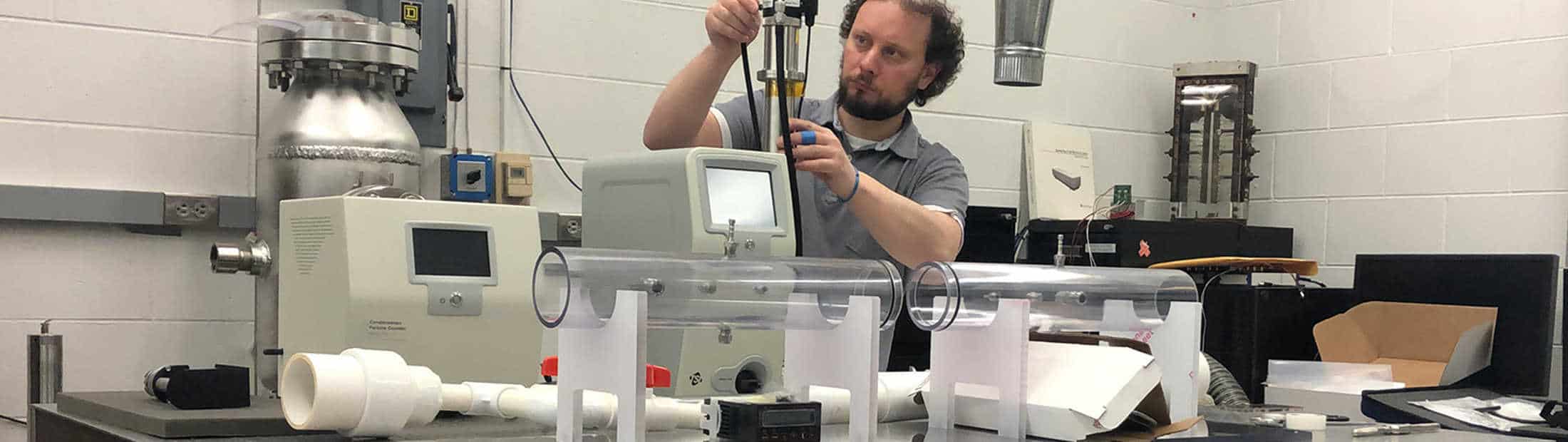
Clack and Gamba began testing N95 masks in March as part of a larger effort between Michigan Engineering and Michigan Medicine to determine how to disinfect N95 masks for reuse. The team created a small wind tunnel in the lab to test mask integrity after decontamination procedures. They fired an air stream of fine particles at the masks and measured the percentage that passed through.
Since those early days, the team has added to its testing toolkit. Funding from the Battle Creek-based LaTour Family Foundation, Michigan Engineering and Michigan Medicine allowed the researchers to add a scanning mobility particle size spectrometer to test masks for particle filtration.

In addition, the team has built its own equipment to test liquid penetration and breathability. The apparatus can mimic real world conditions, such as a spurt of blood, by firing slugs of fluid at masks to measure penetration.
“Surgical masks are in high demand right now within the hospital systems for workers as well as visitors since N95 masks are still going to frontline medical personnel,” Gamba said. “Just like N95s, we don’t have enough surgical masks in the U.S. and we’re acquiring imported and domestic masks without knowing the quality of what we’re bringing in.
“So there is a need for us to evaluate what’s out there for surgical-like masks or off-brand name products because, in this situation, they often don’t come from regular suppliers.”
This effort is a result of a partnership between the College and Michigan Medicine to identify problems and assign U-M engineers to address them. Deactivating viruses on N95 masks is among the first, most-pressing issues doctors on this COVID-19 Rapid Response Steering Committee identified.